Impaled, 1 foot piece of shrapnel in right eye: Respirations 14: Female six months pregnant; broken left, lower leg: Respirations. Snap a photo to screen for thousands of skin conditions and symptoms using artificial intelligence. Procalcitonin, CRP and leucocyte count were slightly elevated or normal (PCT 0.06 ng/mL CRP 25 mg/L, leucocyte count 9.4 10 3 /microL). In addition to the laboratory data, a final diagnosis of Non‐COVID‐19 Viral was deemed clinically appropriate based on the patient's history of clinical improvement without antibiotics and discharge home. NCCT: 120kV, 280 to 340mA, 5.0 mm slice reconstruction, 1 mm increment; CTA: 100kV, 260 to 300mA, 5.0 mm slice reconstruction, 1 mm increment, 80 mL highly iodinated contrast medium and 50 mL NaCl flush at 4 mL/s; CTP: 80kV, 200 to 250mA, 5 mm slice reconstruction (maximum 10 mm), slice sampling rate 1.50 s (minimum 1.33 s), scan time 45 s.
You are here:Home >Burn Triage and Treatment - Thermal Injuries Taskpaper – plain text to do lists 3 5 1.
General Information
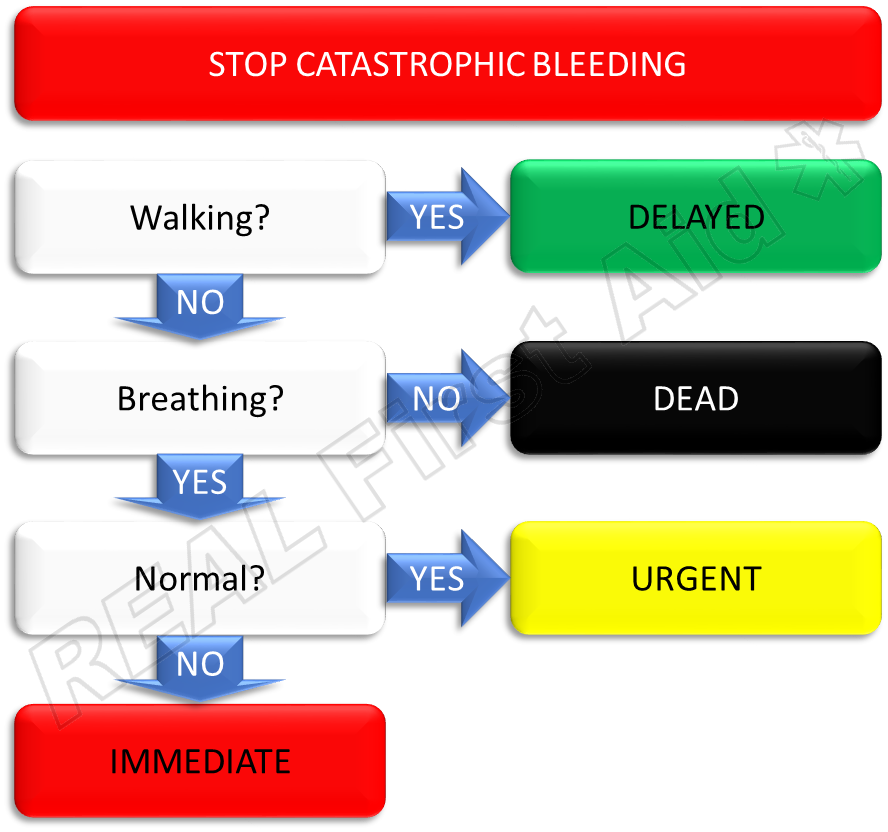
Triage 1 0 14 Ml =
- After a chemical mass casualty incident, trauma with or without burns is expected to be common.
- Burn therapy adds significant logistical requirements and complexity to the medical response in a chemical mass casualty incident.
- Burns complicating physical injury and/or chemical injury decrease the likelihood of survival.
- Health care providers with burn expertise are needed to optimize burn care.
- Consultation with American Burn Association Verified Burn Centers is recommended
Diagnosis of Burns
- Definition: A burn is the partial or complete destruction of skin caused by some form of energy, usually thermal energy.
- Burn severity is dictated by:
- Percent total body surface area (TBSA) involvement
- Burns >20-25% TBSA require IV fluid resuscitation
- Burns >30-40% TBSA may be fatal without treatment
- In adults: 'Rule of Nines' is used as a rough indicator of % TBSA
Rule of Nines for Establishing Extent of Body Surface BurnedAnatomic Surface % of total body surface Head and neck 9% Anterior trunk 18% Posterior trunk 18% Arms, including hands 9% each Legs, including feet 18% each Genitalia 1% - In children, adjust percents because they have proportionally larger heads (up to 20%) and smaller legs (13% in infants) than adults
- Lund-Browder diagrams improve the accuracy of the % TBSA for children.
- Palmar hand surface is approximately 1% TBSA
Estimating Percent Total Body Surface Area in Children Affected by Burns
(A) Rule of 'nines'
(B) Lund-Browder diagram for estimating extent of burns
(Adapted from The Treatment of Burns, edition 2, Artz CP and Moncrief JA, Philadelphia, WB Saunders Company, 1969)
- Depth of burn injury (deeper burns are more severe)
- Superficial burns (first-degree and superficial second-degree burns)
- First-degree burns
- Damage above basal layer of epidermis
- Dry, red, painful ('sunburn')
- Second-degree burns
- Damage into dermis
- Skin adnexa (hair follicles, oil glands, etc,) remain
- Heal by re-epithelialization from skin adnexa
- The deeper the second-degree burn, the slower the healing (fewer adnexa for re-epithelialization)
- Moist, red, blanching, blisters, extremely painful
- Superficial burns heal by re-epithelialization and usually do not scar if healed within 2 weeks
- First-degree burns
- Deep burns (deep second-degree to fourth-degree burns)
- Deep second-degree burns (deep partial-thickness)
- Damage to deeper dermis
- Less moist, less blanching, less pain
- Heal by scar deposition, contraction and limited re-epithelialization
- Third-degree burns (full-thickness)
- Entire thickness of skin destroyed (into fat)
- Any color (white, black, red, brown), dry, less painful (dermal plexus of nerves destroyed)
- Heal by contraction and scar deposition (no epithelium left in middle of wound)
- Fourth-degree burns
- Burn into muscle, tendon, bone
- Need specialized care (grafts will not work)
- Deep burns usually need skin grafts to optimize results and lead to hypertrophic (raised) scars if not grafted
- Deep second-degree burns (deep partial-thickness)
- Superficial burns (first-degree and superficial second-degree burns)
- Age
- Mortality for any given burn size increases with age
- Children/young adults can survive massive burns
- Children require more fluid per TBSA burns
- Elderly may die from small (<15% TBSA) burns
- Children/young adults can survive massive burns
- Mortality for any given burn size increases with age
- Smoke inhalation injury
- Smoke inhalation injury doubles the mortality relative to burn size
- Associated injuries
- Other trauma increases severity of injury
- Delay in resuscitation
- Delay increases fluid requirements
- Need for escharotomies and fasciotomies
- Increases fluid requirements
- Use of alcohol or drugs (especially methamphetamine)
- Makes resuscitation more difficult
- Percent total body surface area (TBSA) involvement
American Burn Association Burn Unit Referral Criteria *
*Criteria not established for very large mass casualty incidents (MCI)
Summary of Burn Unit Referral Criteria (PDF - 7 KB) (American Burn Association)
- Second- and third-degree burns greater than 10% TBSA in patients under 10 or over 50 years of age
- Second- and third-degree burns greater than 20% TBSA in other age groups
- Second- and third-degree burns that involve the face, hands, feet, genitalia, perineum, and major joints
- Third-degree burns greater than 5% TBSA in any age group
- Electrical burns, including lightning injury
- Chemical burns
- Inhalation injury
- Burn injury in patients with pre-existing medical disorders that could complicate management, prolong recovery, or affect mortality (e.g., significant chemical exposure)
- Any patients with burns and concomitant trauma (e.g., fractures, blast injury) where burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, the patient may be treated initially in a trauma center until stable before being transferred to a burn center. Physician judgment will be necessary in such situations and should be in concert with the regional medical control plan and triage protocols appropriate for the incident
- Hospitals without qualified personnel or equipment for the care of children should transfer children with burns to a Verified Burn Center with these capabilities
- Burn injury in children who will require special social/emotional and/or long-term rehabilitative support, including cases involving suspected child abuse or substance abuse
Treatment
- General information
- All burn patients should initially be treated with the principles of Advanced Burn and/or Trauma Life Support
- The ABC's (airway, breathing, circulation) of trauma take precedent over caring for the burn
- Search for other signs of trauma
- All burn patients should initially be treated with the principles of Advanced Burn and/or Trauma Life Support
- Verified Burn Centers provide advanced support for complex cases
- Certified by the American College of Surgeons (ACS) Committee on Trauma and the American Burn Association (ABA)
- Resources will give advice or assist with care
- Burn Unit Referral Criteria (PDF - 7 KB) (American Burn Association)
- Airway
- Extensive burns may lead to massive edema
- Obstruction may result from upper airway swelling
- Risk of upper airway obstruction increases with
- Massive burns
- All patients with deep burns >35-40% TBSA should be endotracheally intubated
- Burns to the head
- Burns inside the mouth
- Massive burns
- Intubate early if massive burn or signs of obstruction
- Intubate if patients require prolonged transport and any concern with potential for obstruction
- If any concerns about the airway, it is safer to intubate earlier than when the patient is decompensating
- Signs of airway obstruction
- Hoarseness or change in voice
- Use of accessory respiratory muscles
- High anxiety
- Tracheostomies not needed during resuscitation period
- Remember: Intubation can lead to complications, so do not intubate if not needed
- Breathing
- Hypoxia
- Fire consumes oxygen so people may suffer from hypoxia as a result of flame injuries
- Carbon monoxide (CO)
- Byproduct of incomplete combustion
- Binds hemoglobin with 200 times the affinity of oxygen
- Leads to inadequate oxygenation
- Diagnosis of CO poisoning
- Nondiagnostic
- PaO2 (partial pressure of O2 dissolved in serum)
- Oximeter (difference in oxy- and deoxyhemoglobin)
- Patient color ('cherry red' with poisoning)
- Diagnostic
- Carboxyhemoglobin levels
- <10% is normal
- >40% is severe intoxication
- Carboxyhemoglobin levels
- Nondiagnostic
- Treatment
- Remove source
- 100% oxygen until CO levels are <10%
- Smoke inhalation injury
- Pathophysiology
- Smoke particles settle in distal bronchioles
- Mucosal cells are die
- Sloughing and distal atelectasis
- Increase risk for pneumonia
- Diagnosis
- History of being in a smoke-filled enclosed space
- Bronchoscopy
- Soot beneath the glottis
- Airway edema, erythema, ulceration
- Nondiagnostic clinical tests
- Early chest x-ray
- Early blood gases
- Nondiagnostic clinical findings
- Soot in sputum or saliva
- Singed facial hair
- Treatment
- Supportive pulmonary management
- Aggressive respiratory therapy
- Pathophysiology
- Hypoxia
- Circulation
- Obtain IV access anywhere possible
- Unburned areas preferred
- Burned areas acceptable
- Central access more reliable if proficient
- Cut-downs are last resort
- Resuscitation in burn shock (first 24 hours)
- Massive capillary leak occurs after major burns
- Fluids shift from intravascular space to interstitial space
- Fluid requirements increase with greater severity of burn (larger % TBSA, increase depth, inhalation injury, associate injuries - see above)
- Fluid requirements decrease with less severe burn (may be less than calculated rate)
- IV fluid rate dependent on physiologic response
- Place Foley catheter to monitor urine output
- Goal for adults: urine output of 0.5 ml/kg/hour
- Goal for children: urine output of 1 ml/kg/hour
- If urine output below these levels, increase fluid rate
- Preferred fluid: Lactated Ringer's Solution
- Isotonic
- Cheap
- Easily stored
- Resuscitation formulas are just a guide for initiating resuscitation
- Resuscitation formulas:
- Parkland formula most commonly used
- IV fluid - Lactated Ringer's Solution
- Fluid calculation
- 4 x weight in kg x %TBSA burn
- Give 1/2 of that volume in the first 8 hours
- Give other 1/2 in next 16 hours
- Warning: Despite the formula suggesting cutting the fluid rate in half at 8 hours, the fluid rate should be gradually reduced throughout the resuscitation to maintain the targeted urine output, i.e., do not follow the second part of the formula that says to reduce the rate at 8 hours, adjust the rate based on the urine output.
- 4 x weight in kg x %TBSA burn
- Example of fluid calculation
- 100-kg man with 80% TBSA burn
- Parkland formula:
- 4 x 100 x 80 = 32,000 ml
- Give 1/2 in first 8 hours = 16,000 ml in first 8 hours
- Starting rate = 2,000 ml/hour
- Adjust fluid rate to maintain urine output of 50 ml/hr
- Albumin may be added toward end of 24 hours if not adequate response
- Parkland formula most commonly used
- Resuscitation endpoint: maintenance rate
- When maintenance rate is reached (approximately 24 hours), change fluids to D50.5NS with 20 mEq KCl at maintenance level
- Maintenance fluid rate = basal requirements + evaporative losses
- Basal fluid rate
- Adult basal fluid rate = 1500 x body surface area (BSA) (for 24 hrs)
- Pediatric basal fluid rate (<20kg) = 2000 x BSA (for 24 hrs)
- May use
- 100 ml/kg for 1st 10 kg
- 0 ml/kg for 2nd 10 kg
- 20 ml/kg for remaining kg for 24 hrs
- May use
- Evaporative fluid loss
- Adult: (25 + % TBSA burn) x (BSA) = ml/hr
- Pediatric (<20kg): (35 + % TBSA burn) x (BSA) = ml/hr
- Basal fluid rate
- Complications of over-resuscitation
- Compartment syndromes
- Best dealt with at Verified Burn Centers
- If unable to obtain assistance, compartment syndromes may require management
- Limb compartments
- Symptoms of severe pain (worse with movement), numbness, cool extremity, tight feeling compartments
- Distal pulses may remain palpable despite ongoing compartment syndrome (pulse is lost when pressure > systolic pressure)
- Compartment pressure >30 mmHg may compromise muscle/nerves
- Measure compartment pressures with arterial line monitor (place needle into compartment)
- Escharotomies may save limbs
- Performed laterally and medially throughout entire limb
- Performed with arms supinated
- Hemostasis is required
- Fasciotomies may be needed if pressure does not drop to <30 mmHg
- Requires surgical expertise
- Hemostasis is required
- Chest Compartment Syndrome
- Increased peak inspiratory pressure (PIP) due to circumferential trunk burns
- Escharotomies through mid-axillary line, horizontally across chest/abdominal junction
- Abdominal Compartment Syndrome
- Pressure in peritoneal cavity > 30 mmHg
- Measure through Foley catheter
- Signs: increased PIP, decreased urine output despite massive fluids, hemodynamic instability, tight abdomen
- Treatment
- Abdominal escharotomy
- NG tube
- Possible placement of peritoneal catheter to drain fluid
- Laparotomy as last resort
- Pressure in peritoneal cavity > 30 mmHg
- Acute Respiratory Distress Syndrome (ARDS)
- Increased risk and severity if over-resuscitation
- Treatment supportive
- Compartment syndromes
- Obtain IV access anywhere possible
- Wound Care
- During initial or emergent care, wound care is of secondary importance
- Advanced Burn Life Support recommendations
- Cover wound with clean, dry sheet or dressing. NO WET DRESSINGS.
- Simple dressing if being transported to burn center (they will need to see the wound)
- Sterile dressings are preferred but not necessary
- Covering wounds improves pain
- Elevate burned extremities
- Maintain patient's temperature (keep patient warm)
- While cooling may make a small wound more comfortable, cooling any wound >5% TBSA will cool the patient
- Cover wound with clean, dry sheet or dressing. NO WET DRESSINGS.
- If providing prolonged care
- Wash wounds with soap and water (sterility is not necessary)
- Maintain temperature
- Topical antimicrobials help prevent infection but do not eliminate bacteria
- Silver sulfadiazine for deep burns
- Bacitracin and nonsticky dressings for more superficial burns
- Skin grafting
- Deep burns require skin grafting
- Grafting may not be necessary for days
- Preferable to refer patients with need for grafting to Verified Burn Centers or, if not available, others trained in surgical techniques
- Grafting of extensive areas may require significant amounts of blood
- Patient's temperature must be watched
- Anesthesia requires extra attention
- Medications
- All pain meds should be given IV
- Tetanus prophylaxis should be given as appropriate
- Prophylactic antibiotics are contraindicated
- Systemic antibiotics are only given to treat infections
Special Burns
- General information
- Often require specialized care
- Calling a Verified Burn Center is advised
- Electrical injuries
- Extent of injury may not be apparent
- Damage occurs deep within tissues
- Damage frequently progresses
- Electricity contracts muscles, so watch for associated injuries
- Cardiac arrhythmias may occur
- If arrhythmia present, patient needs monitoring
- CPR may be lifesaving
- Myoglobinuria may be present
- Color best indicator of severity
- If urine is dark (black, red), myoglobinuria needs to be treated
- Increase fluids to induce urine output of 75-100 ml/hr in adults
- In children, target urine output of 2 ml/kg/hour
- Alkalinize urine (give NaHCOi3)
- Check for compartment syndromes
- Mannitol as last resort
- Compartment syndromes are common
- Long-term neuro-psychiatric problems may result
- Extent of injury may not be apparent
- Chemical Burns
- Brush off powder
- Prolonged irrigation required
- Do not seek antidote
- Delays treatment
- May result in heat production
- Special chemical burns require contacting a Verified Burn Center, for example:
- Hydrofluoric acid burn
American Burn Association Information
- The American Burn Association (ABA) is an organization of burn caregivers who have set up a network to assist with management of burn disasters.
- The ABA has set up a system to verify burn centers (similar to Verified Trauma Centers) as meeting standards for managing patients with burns of all types of severity.
- Verified Burn Centers participate in disaster planning and have set up a network for transporting burn patients throughout the country.
- Verified Burn Centers are always available for advice and assistance in managing burn patients.
- To find the nearest Verified Burn Center near you,
- contact the ABA Web site: www.ameriburn.org or
- e-mail: info@ameriburn.org or
- call: 312-642-9260
- The ABA offers ABA Advanced Burn Life Support (ABLS), a Self-directed, Web-based Learning Program.
Acknowledgement: This CHEMM Web page was adapted from REMM and prepared in consultation with Dr. David Greenhalgh, President of the American Burn Association, August 2006
- Greenwood JE. Burn injury and explosions: an Australian perspective. Eplasty. 2009 Sep 16;9:e40. [PubMed Citation]
- Orgill DP. Excision and skin grafting of thermal burns. N Engl J Med. 2009 Feb 26;360(9):893-901. [PubMed Citation]
- Holmes JH 4th. Critical issues in burn care. J Burn Care Res. 2008 Nov-Dec;29(6 Suppl 2):S180-7. [PubMed Citation]
- Singer AJ, Dagum AB. Current management of acute cutaneous wounds. N Engl J Med. 2008 Sep 4;359(10):1037-46. [PubMed Citation]
- White CE, Renz EM. Advances in surgical care: management of severe burn injury. Crit Care Med. 2008 Jul;36(7 Suppl):S318-24. [PubMed Citation]
- Yurt RW, Lazar EJ, Leahy NE, Cagliuso NV Sr, Rabbitts AC, Akkapeddi V, Cooper A, Dajer A, Delaney J, Mineo FP, Silber SH, Soloff L, Magbitang K, Mozingo DW. Burn disaster response planning: an urban region's approach. J Burn Care Res. 2008 Jan-Feb;29(1):158-65. [PubMed Citation]
- Barillo DJ, Wolf S. Planning for burn disasters: lessons learned from one hundred years of history. J Burn Care Res. 2006 Sep-Oct;27(5):622-34. [PubMed Citation]
- Saffle JR, Gibran N, Jordan M. Defining the ratio of outcomes to resources for triage of burn patients in mass casualties. J Burn Care Rehabil, 2005 Nov-Dec;26(6):478-82 [PubMed Citation]
- Allison K, Porter K. Consensus on the pre-hospital approach to burns patient management. Injury. 2004 Aug;35(8):734-8. [PubMed Citation]
- Ahuja RB, Bhattacharya S. Burns in the developing world and burn disasters. BMJ. 2004 Aug 21;329(7463):447-9. [PubMed Citation]
- Sheridan RL. Burns. Crit Care Med. 2002 Nov;30(11 Suppl):S500-14. [PubMed Citation]
- Herndon DN, ed. Total Burn Care (2nd Ed), WB Saunders, London, 2002.
- Leslie CL, Cushman M, McDonald GS, Joshi W, Maynard AM. Management of multiple burn casualties in a high volume ED without a verified burn unit. Am J Emerg Med. 2001 Oct;19(6):469-73. [PubMed Citation]
- Mackie DP, Koning HM. Fate of mass burn casualties: implications for disaster planning. Burns. 1990 Jun;16(3):203-6. [PubMed Citation]
Screenflick 2 2 17 – capture screen movement to video. PDF documents can be viewed with the free Adobe® Reader™
- Second- and third-degree burns greater than 10% TBSA in patients under 10 or over 50 years of age
- Second- and third-degree burns greater than 20% TBSA in other age groups
- Second- and third-degree burns that involve the face, hands, feet, genitalia, perineum, and major joints
- Third-degree burns greater than 5% TBSA in any age group
- Electrical burns, including lightning injury
- Chemical burns
- Inhalation injury
- Burn injury in patients with pre-existing medical disorders that could complicate management, prolong recovery, or affect mortality (e.g., significant chemical exposure)
- Any patients with burns and concomitant trauma (e.g., fractures, blast injury) where burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, the patient may be treated initially in a trauma center until stable before being transferred to a burn center. Physician judgment will be necessary in such situations and should be in concert with the regional medical control plan and triage protocols appropriate for the incident
- Hospitals without qualified personnel or equipment for the care of children should transfer children with burns to a Verified Burn Center with these capabilities
- Burn injury in children who will require special social/emotional and/or long-term rehabilitative support, including cases involving suspected child abuse or substance abuse
Treatment
- General information
- All burn patients should initially be treated with the principles of Advanced Burn and/or Trauma Life Support
- The ABC's (airway, breathing, circulation) of trauma take precedent over caring for the burn
- Search for other signs of trauma
- All burn patients should initially be treated with the principles of Advanced Burn and/or Trauma Life Support
- Verified Burn Centers provide advanced support for complex cases
- Certified by the American College of Surgeons (ACS) Committee on Trauma and the American Burn Association (ABA)
- Resources will give advice or assist with care
- Burn Unit Referral Criteria (PDF - 7 KB) (American Burn Association)
- Airway
- Extensive burns may lead to massive edema
- Obstruction may result from upper airway swelling
- Risk of upper airway obstruction increases with
- Massive burns
- All patients with deep burns >35-40% TBSA should be endotracheally intubated
- Burns to the head
- Burns inside the mouth
- Massive burns
- Intubate early if massive burn or signs of obstruction
- Intubate if patients require prolonged transport and any concern with potential for obstruction
- If any concerns about the airway, it is safer to intubate earlier than when the patient is decompensating
- Signs of airway obstruction
- Hoarseness or change in voice
- Use of accessory respiratory muscles
- High anxiety
- Tracheostomies not needed during resuscitation period
- Remember: Intubation can lead to complications, so do not intubate if not needed
- Breathing
- Hypoxia
- Fire consumes oxygen so people may suffer from hypoxia as a result of flame injuries
- Carbon monoxide (CO)
- Byproduct of incomplete combustion
- Binds hemoglobin with 200 times the affinity of oxygen
- Leads to inadequate oxygenation
- Diagnosis of CO poisoning
- Nondiagnostic
- PaO2 (partial pressure of O2 dissolved in serum)
- Oximeter (difference in oxy- and deoxyhemoglobin)
- Patient color ('cherry red' with poisoning)
- Diagnostic
- Carboxyhemoglobin levels
- <10% is normal
- >40% is severe intoxication
- Carboxyhemoglobin levels
- Nondiagnostic
- Treatment
- Remove source
- 100% oxygen until CO levels are <10%
- Smoke inhalation injury
- Pathophysiology
- Smoke particles settle in distal bronchioles
- Mucosal cells are die
- Sloughing and distal atelectasis
- Increase risk for pneumonia
- Diagnosis
- History of being in a smoke-filled enclosed space
- Bronchoscopy
- Soot beneath the glottis
- Airway edema, erythema, ulceration
- Nondiagnostic clinical tests
- Early chest x-ray
- Early blood gases
- Nondiagnostic clinical findings
- Soot in sputum or saliva
- Singed facial hair
- Treatment
- Supportive pulmonary management
- Aggressive respiratory therapy
- Pathophysiology
- Hypoxia
- Circulation
- Obtain IV access anywhere possible
- Unburned areas preferred
- Burned areas acceptable
- Central access more reliable if proficient
- Cut-downs are last resort
- Resuscitation in burn shock (first 24 hours)
- Massive capillary leak occurs after major burns
- Fluids shift from intravascular space to interstitial space
- Fluid requirements increase with greater severity of burn (larger % TBSA, increase depth, inhalation injury, associate injuries - see above)
- Fluid requirements decrease with less severe burn (may be less than calculated rate)
- IV fluid rate dependent on physiologic response
- Place Foley catheter to monitor urine output
- Goal for adults: urine output of 0.5 ml/kg/hour
- Goal for children: urine output of 1 ml/kg/hour
- If urine output below these levels, increase fluid rate
- Preferred fluid: Lactated Ringer's Solution
- Isotonic
- Cheap
- Easily stored
- Resuscitation formulas are just a guide for initiating resuscitation
- Resuscitation formulas:
- Parkland formula most commonly used
- IV fluid - Lactated Ringer's Solution
- Fluid calculation
- 4 x weight in kg x %TBSA burn
- Give 1/2 of that volume in the first 8 hours
- Give other 1/2 in next 16 hours
- Warning: Despite the formula suggesting cutting the fluid rate in half at 8 hours, the fluid rate should be gradually reduced throughout the resuscitation to maintain the targeted urine output, i.e., do not follow the second part of the formula that says to reduce the rate at 8 hours, adjust the rate based on the urine output.
- 4 x weight in kg x %TBSA burn
- Example of fluid calculation
- 100-kg man with 80% TBSA burn
- Parkland formula:
- 4 x 100 x 80 = 32,000 ml
- Give 1/2 in first 8 hours = 16,000 ml in first 8 hours
- Starting rate = 2,000 ml/hour
- Adjust fluid rate to maintain urine output of 50 ml/hr
- Albumin may be added toward end of 24 hours if not adequate response
- Parkland formula most commonly used
- Resuscitation endpoint: maintenance rate
- When maintenance rate is reached (approximately 24 hours), change fluids to D50.5NS with 20 mEq KCl at maintenance level
- Maintenance fluid rate = basal requirements + evaporative losses
- Basal fluid rate
- Adult basal fluid rate = 1500 x body surface area (BSA) (for 24 hrs)
- Pediatric basal fluid rate (<20kg) = 2000 x BSA (for 24 hrs)
- May use
- 100 ml/kg for 1st 10 kg
- 0 ml/kg for 2nd 10 kg
- 20 ml/kg for remaining kg for 24 hrs
- May use
- Evaporative fluid loss
- Adult: (25 + % TBSA burn) x (BSA) = ml/hr
- Pediatric (<20kg): (35 + % TBSA burn) x (BSA) = ml/hr
- Basal fluid rate
- Complications of over-resuscitation
- Compartment syndromes
- Best dealt with at Verified Burn Centers
- If unable to obtain assistance, compartment syndromes may require management
- Limb compartments
- Symptoms of severe pain (worse with movement), numbness, cool extremity, tight feeling compartments
- Distal pulses may remain palpable despite ongoing compartment syndrome (pulse is lost when pressure > systolic pressure)
- Compartment pressure >30 mmHg may compromise muscle/nerves
- Measure compartment pressures with arterial line monitor (place needle into compartment)
- Escharotomies may save limbs
- Performed laterally and medially throughout entire limb
- Performed with arms supinated
- Hemostasis is required
- Fasciotomies may be needed if pressure does not drop to <30 mmHg
- Requires surgical expertise
- Hemostasis is required
- Chest Compartment Syndrome
- Increased peak inspiratory pressure (PIP) due to circumferential trunk burns
- Escharotomies through mid-axillary line, horizontally across chest/abdominal junction
- Abdominal Compartment Syndrome
- Pressure in peritoneal cavity > 30 mmHg
- Measure through Foley catheter
- Signs: increased PIP, decreased urine output despite massive fluids, hemodynamic instability, tight abdomen
- Treatment
- Abdominal escharotomy
- NG tube
- Possible placement of peritoneal catheter to drain fluid
- Laparotomy as last resort
- Pressure in peritoneal cavity > 30 mmHg
- Acute Respiratory Distress Syndrome (ARDS)
- Increased risk and severity if over-resuscitation
- Treatment supportive
- Compartment syndromes
- Obtain IV access anywhere possible
- Wound Care
- During initial or emergent care, wound care is of secondary importance
- Advanced Burn Life Support recommendations
- Cover wound with clean, dry sheet or dressing. NO WET DRESSINGS.
- Simple dressing if being transported to burn center (they will need to see the wound)
- Sterile dressings are preferred but not necessary
- Covering wounds improves pain
- Elevate burned extremities
- Maintain patient's temperature (keep patient warm)
- While cooling may make a small wound more comfortable, cooling any wound >5% TBSA will cool the patient
- Cover wound with clean, dry sheet or dressing. NO WET DRESSINGS.
- If providing prolonged care
- Wash wounds with soap and water (sterility is not necessary)
- Maintain temperature
- Topical antimicrobials help prevent infection but do not eliminate bacteria
- Silver sulfadiazine for deep burns
- Bacitracin and nonsticky dressings for more superficial burns
- Skin grafting
- Deep burns require skin grafting
- Grafting may not be necessary for days
- Preferable to refer patients with need for grafting to Verified Burn Centers or, if not available, others trained in surgical techniques
- Grafting of extensive areas may require significant amounts of blood
- Patient's temperature must be watched
- Anesthesia requires extra attention
- Medications
- All pain meds should be given IV
- Tetanus prophylaxis should be given as appropriate
- Prophylactic antibiotics are contraindicated
- Systemic antibiotics are only given to treat infections
Special Burns
- General information
- Often require specialized care
- Calling a Verified Burn Center is advised
- Electrical injuries
- Extent of injury may not be apparent
- Damage occurs deep within tissues
- Damage frequently progresses
- Electricity contracts muscles, so watch for associated injuries
- Cardiac arrhythmias may occur
- If arrhythmia present, patient needs monitoring
- CPR may be lifesaving
- Myoglobinuria may be present
- Color best indicator of severity
- If urine is dark (black, red), myoglobinuria needs to be treated
- Increase fluids to induce urine output of 75-100 ml/hr in adults
- In children, target urine output of 2 ml/kg/hour
- Alkalinize urine (give NaHCOi3)
- Check for compartment syndromes
- Mannitol as last resort
- Compartment syndromes are common
- Long-term neuro-psychiatric problems may result
- Extent of injury may not be apparent
- Chemical Burns
- Brush off powder
- Prolonged irrigation required
- Do not seek antidote
- Delays treatment
- May result in heat production
- Special chemical burns require contacting a Verified Burn Center, for example:
- Hydrofluoric acid burn
American Burn Association Information
- The American Burn Association (ABA) is an organization of burn caregivers who have set up a network to assist with management of burn disasters.
- The ABA has set up a system to verify burn centers (similar to Verified Trauma Centers) as meeting standards for managing patients with burns of all types of severity.
- Verified Burn Centers participate in disaster planning and have set up a network for transporting burn patients throughout the country.
- Verified Burn Centers are always available for advice and assistance in managing burn patients.
- To find the nearest Verified Burn Center near you,
- contact the ABA Web site: www.ameriburn.org or
- e-mail: info@ameriburn.org or
- call: 312-642-9260
- The ABA offers ABA Advanced Burn Life Support (ABLS), a Self-directed, Web-based Learning Program.
Acknowledgement: This CHEMM Web page was adapted from REMM and prepared in consultation with Dr. David Greenhalgh, President of the American Burn Association, August 2006
- Greenwood JE. Burn injury and explosions: an Australian perspective. Eplasty. 2009 Sep 16;9:e40. [PubMed Citation]
- Orgill DP. Excision and skin grafting of thermal burns. N Engl J Med. 2009 Feb 26;360(9):893-901. [PubMed Citation]
- Holmes JH 4th. Critical issues in burn care. J Burn Care Res. 2008 Nov-Dec;29(6 Suppl 2):S180-7. [PubMed Citation]
- Singer AJ, Dagum AB. Current management of acute cutaneous wounds. N Engl J Med. 2008 Sep 4;359(10):1037-46. [PubMed Citation]
- White CE, Renz EM. Advances in surgical care: management of severe burn injury. Crit Care Med. 2008 Jul;36(7 Suppl):S318-24. [PubMed Citation]
- Yurt RW, Lazar EJ, Leahy NE, Cagliuso NV Sr, Rabbitts AC, Akkapeddi V, Cooper A, Dajer A, Delaney J, Mineo FP, Silber SH, Soloff L, Magbitang K, Mozingo DW. Burn disaster response planning: an urban region's approach. J Burn Care Res. 2008 Jan-Feb;29(1):158-65. [PubMed Citation]
- Barillo DJ, Wolf S. Planning for burn disasters: lessons learned from one hundred years of history. J Burn Care Res. 2006 Sep-Oct;27(5):622-34. [PubMed Citation]
- Saffle JR, Gibran N, Jordan M. Defining the ratio of outcomes to resources for triage of burn patients in mass casualties. J Burn Care Rehabil, 2005 Nov-Dec;26(6):478-82 [PubMed Citation]
- Allison K, Porter K. Consensus on the pre-hospital approach to burns patient management. Injury. 2004 Aug;35(8):734-8. [PubMed Citation]
- Ahuja RB, Bhattacharya S. Burns in the developing world and burn disasters. BMJ. 2004 Aug 21;329(7463):447-9. [PubMed Citation]
- Sheridan RL. Burns. Crit Care Med. 2002 Nov;30(11 Suppl):S500-14. [PubMed Citation]
- Herndon DN, ed. Total Burn Care (2nd Ed), WB Saunders, London, 2002.
- Leslie CL, Cushman M, McDonald GS, Joshi W, Maynard AM. Management of multiple burn casualties in a high volume ED without a verified burn unit. Am J Emerg Med. 2001 Oct;19(6):469-73. [PubMed Citation]
- Mackie DP, Koning HM. Fate of mass burn casualties: implications for disaster planning. Burns. 1990 Jun;16(3):203-6. [PubMed Citation]
Screenflick 2 2 17 – capture screen movement to video. PDF documents can be viewed with the free Adobe® Reader™
Triage 1 0 14 Ml Ounces
'When I lost my cross coverage with another group, I didn't know what to do. Finding TriageLogic literally saved the day. With confident nighttime call coverage, I could focus my efforts on my office and know that my patients were being cared for day and night!'
– Harry A Lehman, III, MD, Pediatrician in Delaware
Our products can provide you with Nurses to Handle Your Patient Calls and Triage Software for your Nurses
Let our nurses answer your patient phone calls. We save you time and ensure that all phone calls are documented
- Schmitt-Thompson Protocols
- All Calls Recorded
- All Licensed Registered Nurses
- Call back time of less than 30 minutes
Schmitt-Thompson powered electronic software for triaging and documenting patient phone calls
- Schmitt-Thompson Protocols
- Works with paper charts or EMR
- Web-based
- Optional patient smart phone app
Improve outcomes for patients with chronic diseases while increasing your revenue and saving time.
- 24/7 nurses to monitor patients
- Custom protocols & orders for the chronic condition of the device
- Option to include non-clinical staff
Triage 1 0 14 Ml Syringe
Find out the steps TriageLogic takes to protect patient data and ensure that our products are properly secure.
Letter from the Medical Director: Technological Advances with TriageLogic
Ravi K Raheja, M.D.
Technology in medicine is evolving faster than most people can keep up. Successful technology companies evolve and create new products that are intuitive and fit into the current infrastructure. Tooth fairy 2 4 4. This approach is known as interoperability, and it allows for progress without drastic change.
Read more here >>

